A Systematic Review of Fish-oil Supplements for the Prevention and Treatment of Hypertension
Abstract
Hypertension is the single biggest cause of various cardiovascular complications and at the same fourth dimension one of the most preventable phenomena. Low- and middle-income countries (LMICs) are facing increasing prevalence of hypertension which is imposing a huge burden on morbidity, premature mortality, and catastrophic health expenditure. This systematic review searched for the nonpharmacological interventions for prevention of hypertension among normotensive people in LMICs considering the menses 1990–2016. This review has been conducted following standard methodology of Cochrane review involving 2 independent reviewers in screening, quality appraisement, and information extraction. Narrative synthesis of included articles was demonstrated using tables and meta-analysis was conducted to puddle the estimates of studies which fulfilled the criteria. Total seven trials were included in the review with 6046 participants from viii LMICs. Ii cluster randomized trials were pooled and there was a statistically meaning consequence (Systolic Blood Pressure: mean difference −2.35 [95% CI: −4.31 to −0.38], Diastolic Blood Pressure: mean difference −two.11 [95% CI: −3.20 to −ane.02]) of home based health education in reducing blood pressure. Iii private studies reported reduction of blood pressure as a result of restricted dietary sodium intake. None of the studies was appraised as low gamble of bias due to poor methodological quality. Non-pharmacological interventions can play important role in preventing the evolution of hypertension among normotensive people. Farther trials with longer follow-up flow and robust methods are recommended for getting stronger evidence on these interventions.
Introduction
Hypertension attributes to the half-dozen% of global burden of diseases and is responsible for 7.seven million global premature deaths annually [1]. Hypertension and its complications alone causes 53% cardiovascular diseases related mortality which is in the long run responsible for most one third of total annual deaths [2]. Due to the epidemiological transition from infectious diseases to noncommunicable diseases (NCDs) and unhealthy sedentary lifestyle, low- and heart-income countries (LMICs) are experiencing the increasing trend of hypertension prevalence [3]. A systematic review and meta-assay estimated that the overall prevalence of hypertension in LMICs is 32.3% [4]. This phenomenon is contributing to the dual burden of both infectious diseases and NCDs in LMICs and at the same fourth dimension imposing the catastrophic healthcare expenditure to the communities and the nations [5].
Despite highly prevalent, hypertension is 1 of the most preventable weather condition [6, 7]. Various studies have demonstrated different lifestyle modification approaches to reduce or foreclose hypertension. Recommended measures for preventing hypertension are reducing body weight in case of obesity, undertaking regular physical action, reduced intake of salt or sodium, increasing potassium supplement, and avoiding harmful use of booze [8]. Dietary intervention such as dietary approaches to stop hypertension has also promisingly reduced blood pressure (BP) [nine]. This specific dietary recommendation included more intake of vegetables and fruits, milk products with lower proportion of fat, reduction of cholesterol, and saturated fatty in meals [nine]. A systematic review synthesizing information from sixteen intervention studies including >3000 participants reported the reduction of both systolic and diastolic BP with increased calcium intake. Reduction of BP was fifty-fifty higher with increasing dose of calcium. Effect of calcium in reducing BP was greater among the younger population [ten]. Complementary and culling medicine has been found useful sometimes in this aspect [11,12,13]. A systematic review incorporated six RCTs and explored the effectiveness of "Yoga" either alone or in combination with conventional therapies in lowering BP. Results from this review also positively associated in reduction of BP although the quality of the included trials was notified as low class [11]. The mind trunk therapy which is a combination of concrete exercise and meditation was examined by one review that included nine RCTs, xiii quasi experimental studies and iv observational studies. Pooled interpretation depicted the significant effect of "Tai Chi"—a martial art originating in aboriginal China, embracing the mind, trunk, and spirit—in reducing BP. Only few of the included RCTs were methodologically strong in this systematic review [12]. An overview of systematic review investigated the event of transcendental meditation—a technique for reducing stress on BP. A total of eight systematic reviews including Cochrane reviews were included. Overall the assessment was fare in terms of the quality of the included reviews. Results from the overview besides supported the function of meditation in lowering BP despite some conflicting results between included reviews [thirteen]. Autonomously from dietary modifications, changing lifestyle, alternative medicine and meditation, therapeutic agent such equally combination of Chlorthalidone and Amiloride have also been tested. This double blinded, placebo controlled randomized trial demonstrates the significance of the therapeutic amanuensis in preventing hypertension [14]. Despite meaning effect on prevention, there is run a risk of experiencing adverse effect among the participants. Taking regular medication for prevention may also heighten question on compliance [xv].
In addition, most of these interventions are based on high-income countries. LMICs are challenged with limited resources to provide useful programs for the early diagnosis, prevention, or control of this huge burden of disease [2, vii, 16]. Interventions for prevention of hypertension among persons with normal BP (Systolic BP (SBP) 120–139 mmHg and diastolic BP (DBP) lxxx–89 mmHg) [17] or prehypertensive (SBP ≥ 120–139 mmHg and/or DBP ≥ 80–89 mmHg) [18] tin can play an important role to tackle this progressively increasing disease and reduce complications and morbidity resulting from that. Our objective of the present systematic review is to explore all available interventions which are nonpharmacological in approach and to synthesize their effectiveness in prevention of hypertension in LMICs.
Methods
This systematic review has been carried out following the methodology of Cochrane systematic reviews [19] and addressed the requirements stated in preferred reporting items for systematic reviews and meta-assay protocols guidelines [twenty, 21]. Details methodology including the development of search strategy, dual-screening process, dual-data extraction, dual appraisal of included articles for quality cess, narrative synthesis, and meta-analysis has been described in the published protocol [22]. A comprehensive search strategy was developed using the key words such as Exercise, "Concrete activity", "Weight loss", "Sodium restriction", "Dietary potassium", "Calcium supplementation", "Fish oil supplementation", Lifestyle, Hypertension, "Blood pressure level" to search different electronic bibliographic database including Embase, MEDLINE through Pubmed, Web of Science, Clinical Trials. gov., the Cochrane Library (Cochrane Central Register of Controlled Trials (Fundamental), Scopus etc. The search period covered from 1990 to 2016. Randomized command trials providing nonpharmacological intervention on normotensive adult population in LMICs were included. Both the screening of "title and abstract" and "full text" of the retrieved articles were conducted independently by ii reviewers and any disagreement was resolved by a third reviewer. Reference management software was used to keep rail of the screening process. Each of the studies was appraised critically for assessment of take a chance of bias (ROB). A narrative synthesis of the characteristics of study participants and types of intervention with specific result was demonstrated. Mean and standard deviation of both systolic and diastolic BP were recorded from baseline and endline information. For meta-analysis, a random effect model was chosen with 95% confidence interval and both the chi squared and I2 statistic were measured. The systematic review is registered in International Prospective Register of Systematic Reviews. Registration number is CRD42017055423.
Results
A total of 5131 articles were retrieved after searching viii selected database using a comprehensive search strategy. Later removing the duplicates, 4093 articles were compiled for title and abstract review. Applying inclusion and exclusion criteria, 19 articles were selected for full text review. We did not found the full text of four articles even after communicating with the respective writer. The main causes of excluding these articles were irrelevance with the review objective. Out of these fifteen manufactures, viii articles were excluded due to the following reasons: four manufactures were not focusing LMIC's; ii articles did not follow RCT pattern; one article was a literature review and intervention was given on hypertensive population in ane article. Subsequently screening, seven RCTs were included in the final assay. The detailed description of the choice procedure of the included articles has been provided in Fig. i using PRISMA flow diagram.
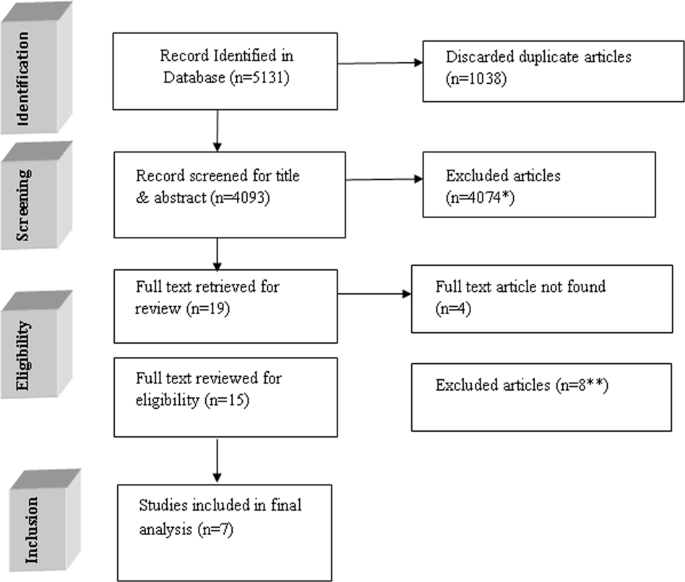
Menses diagram of the inclusion process
Quality assessment of the included studies
We assessed the ROB of the included trials using the guideline of Cochrane review. Bulk of the trials (five out of seven) performed the sequence generation randomly and reported appropriately. Simply three articles described the process of allocation concealment. Thus, at that place was potential take chances of option bias in almost half of the trials. Only ii studies maintained blinding at the level of participants and implementers. Some other two trials mentioned about blinding at the level of outcome assessors. Overall, majority (five in each case) of the trials were unable to minimize the chance of performance bias and detection bias. Almost all the studies mentioned most compunction rate. Merely i study did non describe regarding attrition and marked as unclear data. All the articles were with sufficient information regarding the primary outcome hence nosotros recognized all of them equally at depression risk for selective reporting bias. Majority of the studies did not provide any information regarding other potential biases. We did not get the description regarding contamination in cluster randomized trials and rationale behind the duration of washout menstruation in the studies with crossover design. A graphical sit-in of assessment of ROB has been provided in Figs. ii, 3.
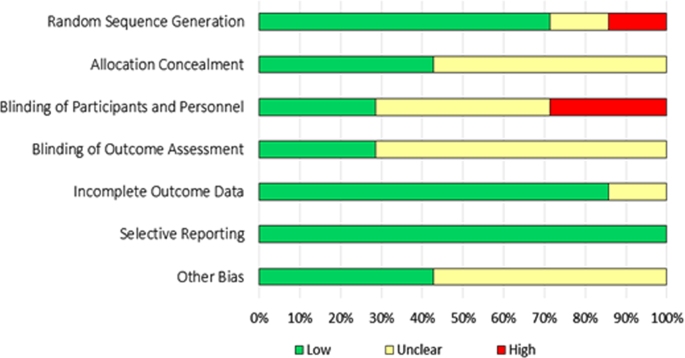
Overall take a chance of bias among the included manufactures
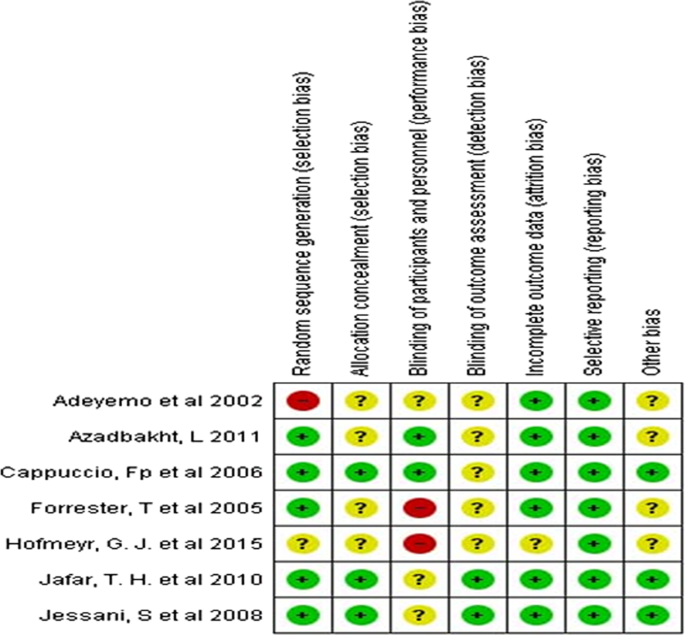
Risk of bias assessment in private studies
A summary description of the basic characteristics of the included manufactures has been given in Table 1. Among the seven included RCTs, two studies used clustered randomized blueprint [23, 24], ii studies were randomized control trials [25, 26] and 3 studies were with crossover design [27,28,29]. Among the 3 crossover trials, two studies incorporated a washout period of 1 and 3 weeks, respectively [28, 29] before altering the treatment options. All the studies described the effectiveness of the intervention to prevent hypertension. The main result, BP, was measured manually with two exceptions which considered both manual and electronic measurements [25, 28]. The interventions provided past different trials were health education plan, soy drink and cow's milk; calcium tablets; and low- or high-salt intake. Among these studies only two met the criteria of meta-assay and rest of the studies were described using summary statistics. All the included studies considered both male and female person except one [26] where intervention was provided among the nonpregnant women. Sample size of the studies varied based on the pattern adapted. Cluster randomized trials included large number of participants [23, 24] whereas some RCTs included <100 participants [25, 27]. 4 studies were conducted in African region [23, 25, 26, 28]; one was in Middle E [27] and 2 studies were conducted in South Asia [24, 29]. All the studies included adult respondents and just one written report included participants anile between 5 and 39 years [24].
Tabular array ii showed the results of studies that were not included in meta-analysis. These studies were heterogeneous plenty for non including in the meta-analysis in terms of interventions, duration of the study, and study settings. Azadbakht et al. measured the beneficial issue of soy milk in comparison with cow's milk on anthropometric measurements and BP for overweight and obese female youths [27]. Information technology showed that the SBP was reduced significantly post-obit the soy beverage intervention menses than that of the cow's milk. Mean percent alter during soy milk period was −0.4 ± 0.9 and −1.7 ± 0.5 during cow'southward milk flow. Diastolic BP was likewise reduced in soy milk drinkable period (−0.4 ± 0.one vs 0.four ± 0.1). Adeyemo et al. provided dietary intervention amid normotensive adults in Southward East Nigeria to determine the feasibility of reducing dietary sodium intake [25]. BP of the participants was measured using both manual procedure and electronic device. In manual measurement, among the participants on low sodium nutrition, SBP was reduced by −4.7 ± ii.viii mmHg for men and past −seven ± four.4 mmHg for women. The diastolic BP was reduced by −1.nine ± 2.ii mmHg amid men and past −1.vi ± 3.four mmHg among women. Hofmeyr et al. explored the consequence of calcium on the BP among nonpregnant women who experienced pre-eclampsia previously [26]. The follow-up was conducted in ii phases at 12 weeks and 24 weeks, respectively. Participants were provided 500 mg calcium tablet each day. Overall, the BP in calcium supplementation grouping was reduced only that was not statistically significant. Forrester et al. compared the effectiveness of high-salt diet (usual diet and additional 50 mEq salt pills) and low-salt diet (usual diet and a reduction of fifty mEq salt) on BP [28]. This report was conducted in two regions of Nigeria and Jamaica and results were compared between these two zones as well. BP was measured using both electronic automated automobile and transmission procedure. The boilerplate upshot from the ii procedures was used in the final analysis. The hateful alter in SBP betwixt low and loftier sodium diet phase was ~five mmHg in both groups. This report depicted that there is a significant efficacy of sodium reduction in lowering the BP. These results were consequent with the studies conducted amidst affluent population in high income countries. Jessani et al. likewise estimated the consequence of high and low sodium diet amongst the Pakistani population [29]. Participants were randomly allocated either in a depression sodium nutrition group (twenty mEq/day) or a high sodium diet grouping (220 mEq/day) for 1 week. The washout catamenia for both the groups was i week before the crossover phase. The crossover catamenia with the altered diet was for some other 1 week. Researchers measured the difference in SBP and diastolic BP in each stage as primary outcome. SBP was classified as high normal SBP and normal SBP. The effect showed that adjusted mean of SBP reduced significantly amidst the participant with high normal SBP (130–139 mmHg) during low sodium diet in comparison with baseline. There were no significant changes among the participants with normal SBP (<130 mmHg) at the baseline.
Meta-analysis
In this analysis, only 2 articles fulfilled the criteria of meta-analysis. Pooled estimate revealed a significant reduction in BP of home based health pedagogy with command (pooled mean departure SBP: −2.35 [95% CI −4.31, −0.38] mmHg, p = 0.02; pooled mean divergence DBP: −ii.11 [95% CI −3.twenty, −1.02] mmHg, p = 0.0001) (Fig. iv). Heterogeneity betwixt these cluster randomized trials was very low (SBP: I 2 = 18%; DBP: I 2 = 0%) which implies that at that place is necessity to conduct meta-analysis without subgroup analysis. The woods plot is demonstrated in Fig. four.
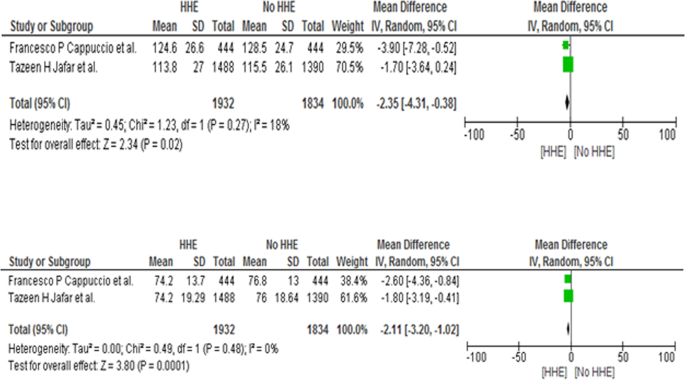
Comparing between dwelling house wellness education (HHE) and no HHE, issue result mean deviation of systolic blood pressure level and diastolic claret pressure
Publication bias
In our review, information technology was not possible to observe the publication bias because of very few numbers of included studies for meta-analysis. Funnel plot generally used to estimate the risk of publication bias. For only two studies, result of this graph is unpredictable. It is also recommended that test of funnel plot asymmetry or being of publication bias is not possible if the selected study is <10 in meta-assay [30].
Discussion
With an aim to examine the effectiveness of nonpharmacological interventions for prevention of hypertension in LMICs, this systematic review included seven trials incorporating 6046 patients from eight countries over the last 16 years. Although a comprehensive search was undertaken, but seven studies met the inclusion criteria. The studies investigated a range of interventions on normotensive population including health education, soy drink, calcium supplementation, and low sodium nutrition. Only of 2 studies were eligible to [23, 24] combine the outcomes through meta-analysis which showed the effects of health education on reducing BP in normotensive participants. The significant alter in BP indicates that positive event of health educational activity amidst normotensive individuals in reducing their BP. However, there were dissimilarities in number and age group among two study participants. Health educational activity for the prevention of hypertension is widely used in the interventions which covered prehypertension individuals. Moreover, this arroyo is also used for normotensive individuals to brand them aware. Study showed that community-based wellness educational activity program on hypertension and cardiovascular hazard factors resulted into declining BP of the participants in the intervention group [31]. The behavior alter communication messages mentioned in the included articles in this review focused on knowledge of lifestyle modification such equally lowering common salt intake in food [23], increased concrete activity, cessation of smoking, consumption of low fat diet including dairy products, and increased intake of fruits and vegetables [24]. Some other systematic review demonstrated the effectiveness of lifestyle modification on metabolic syndrome where information from 8 trials were pooled together [32].
In this review, 3 studies reported issue on reducing BP through reduction in dietary sodium intake [25, 28, 29]. Intervention period in these studies were short, ranging from two to viii weeks. The effect showed significant effect of sodium intake modification, it is worth mentioning that the 3 included studies varied in their findings, reporting different range of changes in SBP and DBP. A Cochrane review too demonstrated the meaning alter in BP among White, Blackness, and Asian people with normal BP where there was a greater reduction charge per unit amid Blackness and Asian people [33].
One RCT (crossover pattern) focused on the effect of soy drinks and moo-cow milk among the females [27]. SBP reduced significantly but no significant changes in DBP due to the intervention of soy potable. However, included participants were obese and on a weight reducing diet. Calcium tablet was given to intervention group in one written report [26] where no significant change in reducing BP was observed. Like results has been demonstrated in a systematic review incorporating 16 trials [10] where slight reduction of BP was observed due to increase in dietary calcium intake. Still, these trials could not conclude with strong recommendations for this specific intervention.
As per world wellness system, sodium reduction in nutrient intake can reduce BP in normotensive individuals [two]. In this systematic review, a trend toward reduction in BP was observed past dietary sodium reduction. Studies conducted by Law et al. and Miller et al. [34, 35] reveled that participants having higher BP at baseline resulted in greater reductions in BP due to the event of sodium reduction. Many studies demonstrated that decreasing sodium in diets accept benefits in lowering BP among prehypertensive participants [36,37,38]. Yet, 1 report showed that the reduction of dietary sodium has no significant effect in normotensive individuals with SBP < 130 mmHg and with normal kidney part [39]. Another crossover study reported no significant changes in BP due to the reduction of salt intake [40].
No studies on physical activities related intervention to reduce hypertension was found in LMICs. However, meta-analysis of seven studies conducted among Brazilian population likewise demonstrated the significant impact of resistance practise and aerobics in lowering both SBP and DBP [41]. Pooled estimate showed reduction in both systolic and diastolic pressures which was statistically significant. But the sample size of included studies were very pocket-size with brusque intervention period and both normotensive and hypertensive patients were included. Some other systematic review and meta-assay conducted demonstrated that isometric handgrip do is efficacious for reducing SBP and DBP in developed participants [42].
We conducted a broad search of several databases but placed restrictions on the language of the study when searching the electronic databases. Studies published in english language were merely considered in this review which is one of the main limitations. It is likely that there are other studies published in other languages which we take missed in this review. Strengths of this systematic review are the inclusion of RCTs only and post-obit Cochrane guideline strictly.
None of the included studies was institute as low ROB and also methodologically none of the studies was of high quality. In some studies, brusk duration of intervention catamenia with minor sample demonstrated quick significant results but their sustainability remained questionable. Follow-up after a longer duration could have observed for the sustainability of the bear on of interventions. Studies did not mention most potential confounders and contamination in case of cluster randomized trials.
Conclusion
This review demonstrated the effectiveness of nonpharmacological interventions for prevention of hypertension of the included trials. Given the limited scientific evidence in LMICs and quality of the evidences, no potent conclusion nigh effectiveness of nonpharmacological approaches could be drawn. This systematic review highlights the need of future enquiry opportunities and a necessity for more scientific studies with larger numbers of participants and longer intervention menses using robust study pattern.
Summary
What is known nigh topic
-
Hypertension attributes to the cardiovascular disease burden and responsible for premature death.
-
Different not pharmacological approaches have been implemented for prevention of hypertension in loftier income countries
What this study adds
-
Explored all bachelor non pharmacological intervention trials in LMICs
-
Dwelling based health education has got pregnant result in preventing hypertension among people with normal blood pressure level in LMICs
-
More researches with robust methodology and longer follow up are required for recommending other non pharmacological approaches
Data availability
The datasets generated and/or analyzed during in this review shall be available from the corresponding author on reasonable asking.
References
-
Forouzanfar MH, Liu P, Roth GA, Ng Yard, Biryukov S, Marczak Fifty, et al. Global burden of hypertension and systolic claret force per unit area of at least 110–115 mmhg, 1990–2015. JAMA. 2017;317:165–82.
-
WHO. A global brief on hypertension: silent killer, global public wellness crisis: Earth Wellness Twenty-four hours 2013. World Health Arrangement. 2013.
-
Mackay J, Mensah Yard, Mendis S, Greenlund K. The atlas of heart disease and stroke. Geneva, Switzerland: World Wellness Organisation; 2004.
-
Sarki AM, Nduka CU, Stranges S, Kandala Due north-B, Uthman OA. Prevalence of hypertension in low-and middle-income countries: a systematic review and meta-analysis. Medicine. 2015;94:e1959.
-
Si Y, Zhou Z, Su M, Ma M, Xu Y, Heitner J. Catastrophic healthcare expenditure and its inequality for households with hypertension: evidence from the rural areas of Shaanxi Province in Prc. Int J Equity Health. 2017;sixteen:27.
-
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23.
-
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya Yard, Adair-Rohani H, et al. A comparative take a chance assessment of burden of disease and injury owing to 67 gamble factors and risk factor clusters in 21 regions, 1990–2010: a systematic assay for the Global Burden of Affliction Study 2010. Lancet. 2012;380:2224–60.
-
Slama M, Susic D, Frohlich ED. Prevention of hypertension. Curr Opin Cardiol. 2002;17:531–6.
-
Appel LJ, Brands MW, Daniels SR, Karanja Due north, Elmer PJ, Sacks FM. Dietary approaches to prevent and care for hypertension: a scientific statement from the American Eye Clan. Hypertens. 2006;47:296–308.
-
Cormick G, Ciapponi A, Cafferata ML, Belizan JM. Calcium supplementation for prevention of primary hypertension. Cochrane Database Syst Rev. 2015;30:Cd010037.
-
Wang J, Xiong X, Liu West. Yoga for essential hypertension: a systematic review. PLoS I. 2013;eight:e76357.
-
Yeh GY, Wang C, Wayne PM, Phillips RS. The effect of tai chi exercise on blood force per unit area: a systematic review. Prev Cardiol. 2008;11:82–9.
-
Ooi SL, Giovino Thousand, Pak SC. Transcendental meditation for lowering blood force per unit area: an overview of systematic reviews and meta-analyses. Complement Ther Med. 2017;34:26–34.
-
Fuchs SC, Poli‐de‐Figueiredo CE, Figueiredo Neto JA, Scala LCN, Whelton PK, Mosele F, et al. Effectiveness of chlorthalidone plus amiloride for the prevention of hypertension: the PREVER‐prevention randomized clinical trial. J Am Center Assoc. 2016;5:e004248.
-
Sabaté East. Adherence to long-term therapies: evidence for action. Switzerland: World Health Organization; 2003.
-
Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380:611–9.
-
Gabb GM, Mangoni A, Anderson CS, Cowley D, Dowden JS, Golledge J, et al. Guideline for the diagnosis and management of hypertension in adults—2016. Med J Aust. 2016;205:85–9.
-
Chia Y. Prehypertension: what Is the electric current status? Malays Fam Physician. 2008;three:72.
-
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version five.one.0. England: The Cochrane Collaboration; 2011.
-
Moher D, Shamseer 50, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-assay protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
-
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew One thousand, et al. Preferred reporting items for systematic review and meta-assay protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
-
Saif-Ur-Rahman KM, Hasan M, Hossain Southward, Shafique S, Khalequzzaman Thou, Haseen F, et al. Non-pharmacological interventions for the prevention of hypertension in low-income and center-income countries: protocol for a systematic review and meta-assay. BMJ Open. 2018;8:e020724.
-
Cappuccio FP, Kerry SM, Micah FB, Plange-Rhule J, Eastwood JB. A community program to reduce common salt intake and blood pressure in Ghana [ISRCTN88789643]. BMC Public Health. 2006;6:13.
-
Jafar TH, Islam Chiliad, Hatcher J, Hashmi Due south, Bux R, Khan A, et al. Community based lifestyle intervention for blood force per unit area reduction in children and young adults in developing land: cluster randomised controlled trial. BMJ. 2010;340:c2641.
-
Adeyemo AA, Prewitt TE, Luke A, Omotade O, Rotimi CN, Brieger West, et al. The feasibility of implementing a dietary sodium reduction intervention amidst free-living normotensive individuals in south west Nigeria. Ethn Dis. 2002;12:207–12.
-
Hofmeyr 1000, Seuc A, Betrán A, Purnat T, Ciganda A, Munjanja S, et al. The effect of calcium supplementation on blood pressure level in not-pregnant women with previous pre-eclampsia: an exploratory, randomized placebo controlled study. Pregnancy Hypertens. 2015;5:273–nine.
-
Azadbakht Fifty, Nurbakhsh S. Issue of soy drink replacement in a weight reducing diet on anthropometric values and blood pressure level among overweight and obese female youths. Asia Pac J Clin Nutr. 2011;20:383–9.
-
Forrester T, Adeyemo A, Soarres-Wynter S, Sargent 50, Bennett F, Wilks R, et al. A randomized trial on sodium reduction in two developing countries. J Hum Hypertens. 2005;19:55–threescore.
-
Jessani S, Hatcher J, Chaturvedi N, Jafar TH. Effect of depression vs. high dietary sodium on blood pressure level levels in a normotensive Indo-Asian population. Am J Hypertens. 2008;21:1238–44.
-
Ioannidis JP, Trikalinos TA. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ. 2007;176:1091–6.
-
Fortmann SP, Winkleby MA, Flora JA, Haskell WL, Taylor CB. Effect of long-term community health didactics on claret pressure and hypertension control: the stanford v-city project. Am J Epidemiol. 1990;132:629–46.
-
Yamaoka K, Tango T. Effects of lifestyle modification on metabolic syndrome: a systematic review and meta-analysis. BMC Med. 2012;x:138.
-
Graudal NA, Hubeck-Graudal T, Jurgens One thousand. Effects of low sodium nutrition versus high sodium diet on claret pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane database Syst Rev. 2017;4:Cd004022.
-
Law M, Frost C, Wald North. By how much does dietary salt reduction lower blood pressure? III-analysis of data from trials of common salt reduction. BMJ. 1991;302:819–24.
-
Miller JZ, Daugherty SA, Weinberger MH, Grim CE, Christian JC, Lang CL. Claret pressure response to dietary sodium brake in normotensive adults. Hypertens. 1983;5:790–5.
-
Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, et al. Long term furnishings of dietary sodium reduction on cardiovascular illness outcomes: observational follow-upwardly of the trials of hypertension prevention (TOHP). BMJ. 2007;334:885.
-
Vasan RS, Sullivan LM, Wilson Pow, Sempos CT, Sundström J, Kannel WB, et al. Relative importance of deadline and elevated levels of coronary heart affliction run a risk factors. Ann Intern Med. 2005;142:393–402.
-
Whelton PK, Appel L, Charleston J, Dalcin AT, Ewart C, Fried L, et al. The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels: results of the Trials of Hypertension Prevention, stage I. JAMA. 1992;267:1213–20.
-
Todd AS, Macginley RJ, Schollum JB, Williams SM, Sutherland WH, Mann JI, et al. Dietary sodium loading in normotensive healthy volunteers does not increment arterial vascular reactivity or claret pressure. Nephrology. 2012;17:249–56.
-
Dickinson KM, Clifton PM, Keogh JB. A reduction of 3 k/24-hour interval from a usual ix g/day salt diet improves endothelial part and decreases endothelin-1 in a randomised cross_over study in normotensive overweight and obese subjects. Atherosclerosis. 2014;233:32–8.
-
Bento VFR, Albino FB, Moura KFd, Maftum GJ, Santos MdCd, Guarita-Souza LC, et al. Impact of physical activity interventions on blood pressure in Brazilian populations. Arq Bras de Cardiol. 2015;105:301–8.
-
Kelley GA, Kelley KS. Isometric handgrip exercise and resting blood force per unit area: a meta-analysis of randomized controlled trials. J Hypertens. 2010;28:411–viii.
Funding
At that place is no external funding for this systematic review. This review has been conducted by the Systematic Review Centre (SRC) of Department of Public Wellness and Informatics at Bangabandhu Sheikh Mujib Medical University (BSMMU), Bangladesh which has been established with the support of SHARE (Strengthening Health Applying Research Testify) project of icddr,b funded past the European Union (Grant Contract No DCI-SANTE/2014/342-479). icddr,b acknowledges with gratitude the commitment of Eu (EU) to its inquiry efforts. icddr,b is also grateful to the Governments of Bangladesh, Canada, Sweden and the UK for providing core/unrestricted support.
Author contributions
KMSUR, IA, SH, MH, and SI conceptualized the review in consultation with the co-reviewers. KMSUR wrote the get-go typhoon of this manuscript with substantial inputs from MH and RM. KMSUR, MH, and AM performed to the literature search. Screening, collection, and analysis of data for all the included interventions were conducted by KMSUR and MH with shut consultation from SH, RM, SS, SI, AR, MK, FH, and IA. All authors provided input, reviewed and finalized the paper before dissemination. The corresponding author is the guarantor of this review. All authors read and approved the concluding manuscript.
Author information
Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of involvement.
Ethics and dissemination
Approval for conducting this systematic review has been taken from the Institutional Review Board (IRB) of Bangabandhu Sheikh Mujib Medical University (BSMMU). No boosted formal ethical assessment and no informed consent are required. Findings of the systematic review will be published in international peer reviewed periodical for dissemination.
Additional data
Publisher's annotation: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution iv.0 International License, which permits utilise, sharing, adaptation, distribution and reproduction in any medium or format, every bit long as you give appropriate credit to the original author(s) and the source, provide a link to the Artistic Commons license, and indicate if changes were made. The images or other third political party fabric in this article are included in the commodity'southward Creative Eatables license, unless indicated otherwise in a credit line to the textile. If material is non included in the article's Creative Eatables license and your intended use is non permitted by statutory regulation or exceeds the permitted use, you lot will need to obtain permission straight from the copyright holder. To view a re-create of this license, visit http://creativecommons.org/licenses/by/4.0/.
Reprints and Permissions
About this article
Cite this article
Saif-Ur-Rahman, K.1000., Shariful Islam, South., Hasan, G. et al. Nonpharmacological interventions for the prevention of hypertension in depression- and middle-income countries: a systematic review and meta-analysis. J Hum Hypertens 33, 786–794 (2019). https://doi.org/10.1038/s41371-019-0223-10
-
Received:
-
Revised:
-
Accepted:
-
Published:
-
Issue Engagement:
-
DOI : https://doi.org/10.1038/s41371-019-0223-x
Source: https://www.nature.com/articles/s41371-019-0223-x
0 Response to "A Systematic Review of Fish-oil Supplements for the Prevention and Treatment of Hypertension"
Enregistrer un commentaire